New FDA-Approved Weight Loss Medications: What You Should Know
New FDA-Approved Weight Loss Medications: What You Should Know
Table of Contents
I. How New Weight Loss Medications Work
II. What to Expect with These Medications
III. Who Can Use the Latest Medications?
IV. Coverage and Costs to Consider
V. Start Your Journey With ScriptsMD
FDA approval for new weight loss medications has brought a wave of attention—and a lot of questions. These treatments aren't magic pills, but can help those facing long-term weight challenges. While traditional methods like diet and exercise remain essential, new medications are adding another layer of support for patients struggling to lose weight on their own.
Whether you're curious about how these drugs work or wondering if one might be right for you, staying informed is key. Each medication comes with its risks, benefits, and guidelines for use. And because they're still new, some details may change as more data becomes available. In this article, we’ll break down the latest weight loss treatment options that have recently earned FDA approval and explain what you should know before starting a conversation with your doctor.
Quick Takeaways
- New FDA-approved medications offer promising results for people struggling with obesity.
- Some treatments mimic natural hormones to help reduce appetite and increase satiety.
- Most medications are prescribed alongside lifestyle changes like diet and exercise.
- Side effects can vary, but common ones include nausea and fatigue
- Insurance coverage may not include all new medications
- Working with a healthcare provider to find the right option is essential.
How New Weight Loss Medications Work
They Target the Body’s Natural Signals
New FDA-approved weight loss medications work differently than older options. Rather than boosting metabolism, they imitate hormones that manage hunger and fullness. Drugs like semaglutide and tirzepatide target brain areas that regulate appetite. This helps people feel satisfied with smaller portions and leads to fewer food cravings. When taken consistently, these medications can noticeably impact eating habits. They’re not designed for cosmetic use but are intended for people with obesity or health issues tied to excess weight, such as high blood pressure or type 2 diabetes.
Timing and Dosage Matter
These medications are usually given through weekly injections, slowly increasing over time. This gradual approach helps reduce the chance of side effects and allows your body to adapt.
- Doctors track your response closely to ensure the medication is safe and effective.
- The dose may be adjusted based on how well you're tolerating it.
This isn’t a short-term fix. It’s part of a more extended plan that includes consistent monitoring, guidance, and lifestyle changes. With patience and medical support, it can be a meaningful part of your weight loss journey.

They’re Used with Lifestyle Changes
The FDA requires these medications to be paired with healthy changes to diet and exercise. On their own, they rarely lead to lasting weight loss. Think of them as a tool, not a cure. Healthcare providers often suggest nutrition counseling or behavioral support alongside treatment. These resources help reinforce better habits and improve results. When combined with consistent effort, the medication can be a strong part of a larger health strategy.
What to Expect with These Medications
Benefits Can Be Significant
In clinical trials, many patients lost 15 to 20 percent of their body weight, often more than with older medications. That kind of weight loss can improve health in noticeable ways.
- Lower risk of heart disease and stroke
- Improved sleep quality and reduced sleep apnea symptoms
- Better blood sugar control in people with type 2 diabetes
- Increased physical mobility and reduced joint pain
People often feel more energized and encouraged to stay on track. These physical and emotional shifts can lead to a cycle of positive habits that reinforce continued progress.
Side Effects Are Common but Often Manageable
Like most medications, these treatments come with potential side effects. Nausea, vomiting, and diarrhea are the most frequently reported, especially during early dose increases. Fatigue and constipation are also reasonably common. These symptoms often ease over time, but staying in contact with your doctor as your body adjusts is essential.
More serious issues, such as pancreatitis, can occur in rare cases. Ongoing medical supervision helps catch problems early and keep treatment on track. Not everyone responds the same way—some may see less weight loss or need to change medications if side effects become too difficult to manage.
Who Can Use the Latest Medications?
Not for Everyone
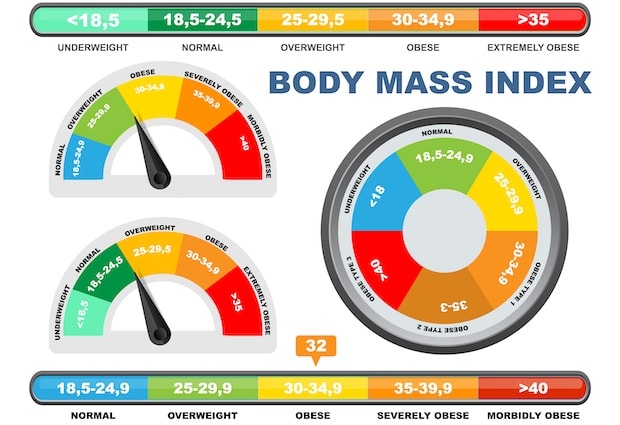
These medications are generally recommended for people with a BMI of 30 or higher. Those with a BMI of 27 and at least one weight-related condition, such as high blood pressure or type 2 diabetes, may also qualify.
Before starting treatment, your doctor will usually:
- Review your complete medical history
- Check for potential conflicts with other medications
- Evaluate whether the benefits outweigh the risks
They are not meant for short-term or cosmetic use. Pregnant individuals or those with certain health conditions may not be eligible. A thorough evaluation ensures the treatment is a safe and appropriate choice.
Working with a Medical Team
Access to these medications often begins with a consultation or referral. Many healthcare systems now use a team-based approach. That team might include doctors, registered dietitians, and behavioral health experts. Each professional supports your success, from monitoring progress to adjusting the plan as your body responds. This structure can make a big difference in staying motivated and on track.
Your doctor is the best place to start if you're considering one of these new treatments. They’ll help assess the medication's safety, discuss possible benefits and risks, and walk you through the next steps. It’s not a one-size-fits-all decision, so having a medical partner to guide the process ensures the approach fits your goals and health history.
Coverage and Costs to Consider
Insurance Isn’t Always Helpful
While these medications have FDA approval, insurance coverage isn’t guaranteed. Some plans may only allow short-term use or require proof that diet and exercise have failed. These policies can create delays or extra steps before starting treatment. Out-of-pocket costs vary widely but can be several hundred dollars a month or more. Before committing, check with your insurer to understand what’s covered. Ask about co-pays, prior authorization requirements, and whether alternative options might be more affordable.
Discount Programs and Alternatives
Some pharmaceutical companies offer savings cards or patient assistance programs, which can significantly lower monthly costs. These programs benefit people without solid insurance coverage or those facing high co-pays.
It’s also smart to ask your provider about:
- Generic or lower-cost versions
- Free samples to try before committing
- Mail-order options that may be cheaper
Cost doesn’t have to be a deal-breaker. Many healthcare teams are familiar with affordability concerns and can suggest ways to make treatment fit your budget while supporting your health goals.
Start Your Journey With ScriptsMD
FDA-approved weight loss medications are offering new hope for those facing long-term challenges with obesity. These treatments are more than quick fixes—they work best when paired with diet, exercise, and medical guidance.
While not ideal for everyone, these medications have helped many achieve sustainable progress. For those who have struggled to lose weight through traditional methods, these medications can provide much-needed support. That said, each case is different. Talking with your doctor about risks, benefits, and long-term goals is essential to making a safe, informed decision.
Want to learn more about the latest weight loss treatment options? Contact ScriptsMD to learn more today.
